
|
|||
|---|---|---|---|
|
|
Hamstring injury in sport Lesiones de los isquiotibiales en el deporte |
|
|
|
Physiotherapy Students University of the La Laguna, Tenerife (Spain) |
Orlando
Pérez San Juan |
|
|
|
Abstract Introduction: The purpose of this article was to assess all the factors involved in the hamstring injury through a brief review. Methods: One database was searched using relevant terms and strategies. Results: Re-injury is reduced with a program of progressive agility and trunk stabilization exercises and icing. The anatomy of the hamstring muscle places it in a vulnerable position during running. Most injuries occur along the proximal musculotendon junction. Discussion: This brief review provides a framework that can be useful for the athletes, coaches, coach fitness, physiotherapist and sport scientist to optimize their work. Keywords: Hamstring injury. Sport.
|
|||
|
|
EFDeportes.com, Revista Digital. Buenos Aires, Año 18, Nº 186, Noviembre de 2013. http://www.efdeportes.com/ |
|
|
1 / 1
Introduction
Hamstring muscle strains are common in sports and often result in chronic pain, recurrent hamstring strains, and reduced sports performance.
Acute hamstring injuries are the most prevalent muscle injuries reported in sport1.
Hamstring injuries occur frequently, with a high recurrence rate, in sports that require maximum sprinting, kicking, acceleration, change of direction or high-speed skilled movements or excessive hip flexion with knee extension.
A previous hamstring injury is the greatest risk factor for a future hamstring injury3,6.
Hamstring strains often are difficult to treat, slow to rehabilitate, and are compounded by a high recurrence rate. Normal recurrence rates are between 12% and 31% within 1 year of returning to sport but may be as high as 54.5%. Factors responsible for the recurrence in hamstring injury include reduced tensile strength of the scar tissue at the site of injury, reduced strength of surrounding musculature as the result of disuse atrophy, reflex inhibition, reduced flexibility of the muscle tendon unit (MTU), and possible adaptive changes in the biomechanics of sporting movements after the original injury2.
Methods
Literature search. The databases PubMed was searched using the terms (Hamstring injury). The reference lists of the articles obtained were searched manually to obtain further studies not identified electronically.
Results
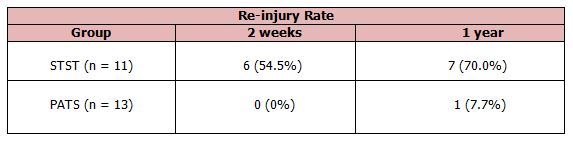
Sherry and Best5 in one study with twenty-four athletes with an acute hamstring strain were randomly assigned to 1 of 2 rehabilitation groups (table 1). Eleven athletes were assigned to a protocol consisting of static stretching, isolated progressive hamstring resistance exercise, and icing (STST group).
Thirteen athletes were assigned to a program consisting of progressive agility and trunk stabilization exercises and icing (PATS group). The number of days for full return to sports, injury recurrence within the first 2 weeks, injury recurrence within the first year of returning to sports, and lower-extremity functional evaluations were collected for all subjects and compared between groups.
Table 1. Incidence of re-injury for the individuals in the stretching and strengthening (STST) group and progressive agility and trunk stabilization (PATS) group
The anatomy of the hamstring muscle places it in a vulnerable position during running. The hamstring muscle is a biarticular muscle, meaning it crosses 2 joints and has 2 major actions (i.e.), hip extension and knee flexion. This also means that the hamstrings are stretched with hip flexion and knee extension. As the lower leg swings forward during the late swing phase of running, the hip flexes and the knee extends simultaneously. Thus, the hamstring muscle becomes actively lengthened to greater than normal lengths6.
Reported causes of hamstring strains include poor lumbar posture, previous injury, lack of flexibility, inadequate warm up, fatigue, strength imbalance, inadequate quadriceps to hamstring ratio, and poor coordination2.
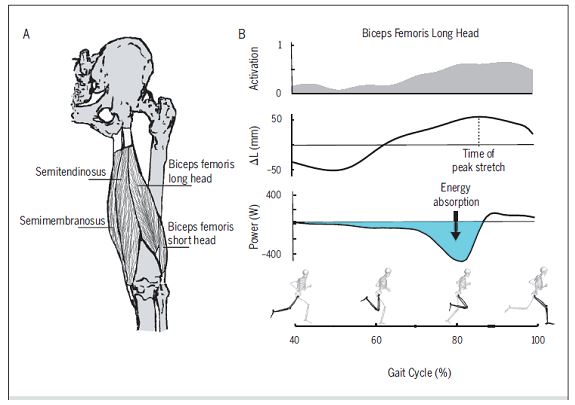
Most hamstring strain injuries happen while running. It is generally believed that they occur during terminal swing phase of the gait cycle. During the second half of the swing, the hamstrings undergo an eccentric contraction and absorb energy from the swing limb before foot contact . Thus, the hamstrings are stretched while subjected to load (eccentric contraction), with the biceps femoral incurring the greatest amount of length change and performing the greatest amount of negative work during this time (Image 1). This may contribute to the tendency of the biceps femoral to be more often injured than the semimembranosus and semitendinosus3.
Image 1. Hamstring in gait cycle
Most hamstring injuries occur along the proximal musculotendon junction (MTJ), where the muscle fibrils intersect with the tendon. Like most acute strain injuries, hamstring strains do not typically involve the muscle tearing away from the tendon.
The healing of soft tissue is characterized by the formation of connective fibrous tissue that is both shorter and less elastic than the original structure, leading to a loss of flexibility and impaired function2.
Early mobilization has been shown to promote collagen penetration and orientation of the regenerating muscle fibers through the scar tissue, as well as recapillarization of the injured area.
Musculoskeletal modelling has recently demonstrated the substantial influence that lumbopelvic muscles can have on the overall stretch of the hamstrings . For example, contralateral hip flexor (i.e., iliopsoas) activity during high-speed running has a large influence on ipsilateral hamstring stretch. That is because activity of the iliopsoas can produce an increase in anterior pelvic tilt during early swing phase, the stretch of the contralateral hamstrings is increased.
The hamstring injuries related to sprint actions affected mainly the proximal part of the biceps femoral, whereas overstretching injuries mainly involved the free proximal portion of the semimembranosus muscle.
It is well accepted that the prevalence of biceps femoral injury is much higher than the medial hamstrings. The elongation peak of the biceps femoral during sprints occurred in the oscillation phase, and to a greater magnitude, with increased speed compared to the medial hamstrings.
The proximal aponeurosis of the biceps femoral is narrower than the distal part, which could explain the finding that fascicle length increases during contraction. Thus, the unique architecture (fascicle length, physiological cross-sectional area, aponeurosis size) of the biceps femoral may explain the greater risk of injury compared to other muscles.
Heiderscheit et al.4 presented evidence that both tendon and muscle remodelling can persist for many months following a hamstring injury.
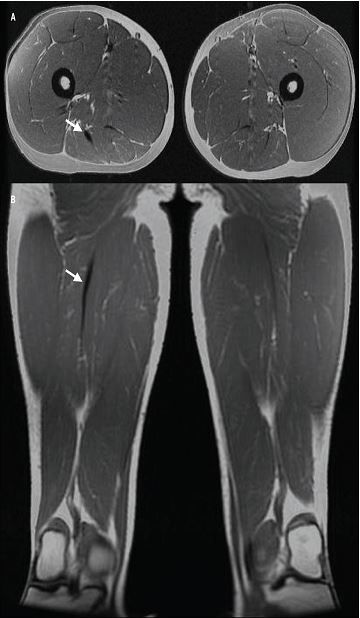
Image 2. Persistent scar tissue, depicted by low-intensity signal (arrow), is evident adjacent to the site
of prior injury along the proximal musculotendon junction of the biceps femoral long head in the (A)
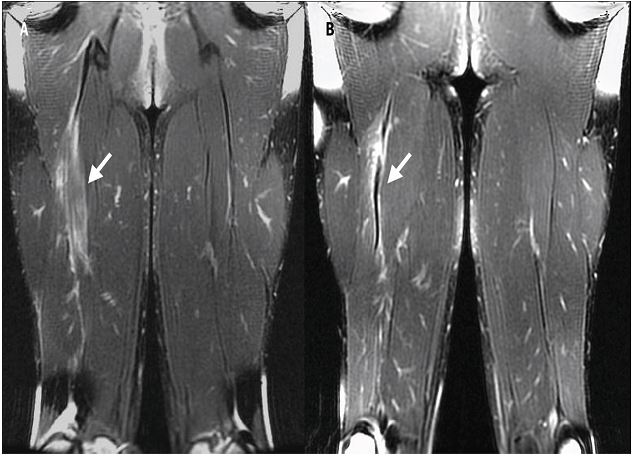
Image 3. T2-weighted coronal images at (A) 10 days and (B) 30 days following injury to the right biceps femoral long head sustained during high-speed running.
Considerable edema and haemorrhage (high-intensity signal) are evident at the site of injury (arrow) on day 10, with persistent fluid remaining at day 30. In addition,
a substantial amount of scar tissue (low-intensity signal) is present by day 30. Of note, this individual was cleared to return to sport 23 days after the injury
Discussion
The purpose of this investigation was to assess all the factors involved in the hamstring injury through a brief review of the literature. This provides a framework that can be useful for the athletes, coaches, coach fitness, physiotherapist and sport scientist to optimize their work.
Future investigations should evaluate the causes of hamstring strains, poor lumbar posture, previous injury, lack of flexibility, inadequate warm up, fatigue, strength imbalance, inadequate quadriceps to hamstring ratio, and poor coordination and others causes undescribed, because despite the advances in knowledge, treatment and physical conditioning plans, the rate is still very high.
References
-
Mendiguchia J, Alentorn-Geli E, Brughelli M. Hamstring strain injuries: are we heading in the right direction? Br J Sports Med., 46 (2):81-5, 2012.
-
Comfort, Paul; Green, Carly M; Matthews, Martyn. Training Considerations after Hamstring Injury in Athletes. Strength & Conditioning Journal. 31 (1):68-74, 2009.
-
Sherry, Marc A; Best, Thomas M; Silder, Amy; Thelen, Darryl G; Heiderscheit, Bryan C. Hamstring Strains: Basic Science and Clinical Research Applications for Preventing the Recurrent Injury. Strength & Conditioning Journal. 33 (3):56-71, 2011.
-
Bryan C. Heiderscheit, Marc A. Sherry, Amy Silder, Elizabeth S. Chumanov, Darryl G. Thelen. Hamstring Strain Injuries: Recommendations for Diagnosis, Rehabilitation, and Injury Prevention. J Orthop Sports Phys Ther; 40 (2):67-81, 2010.
-
Thomas M. Best, Marc A. Sherry. A Comparison of 2 Rehabilitation Programs in the Treatment of Acute Hamstring Strains. J Orthop Sports Phys Ther; 34 (3):116-125, 2004.
-
Brughelli, Matt; Cronin, John. Preventing Hamstring Injuries in Sport. Strength & Conditioning Journal. 30 (1):55-64, 2008.
Another articles in English
 |

Búsqueda personalizada
|
|---|---|
|
EFDeportes.com, Revista
Digital · Año 18 · N° 186 | Buenos Aires,
Noviembre de 2013 |
|